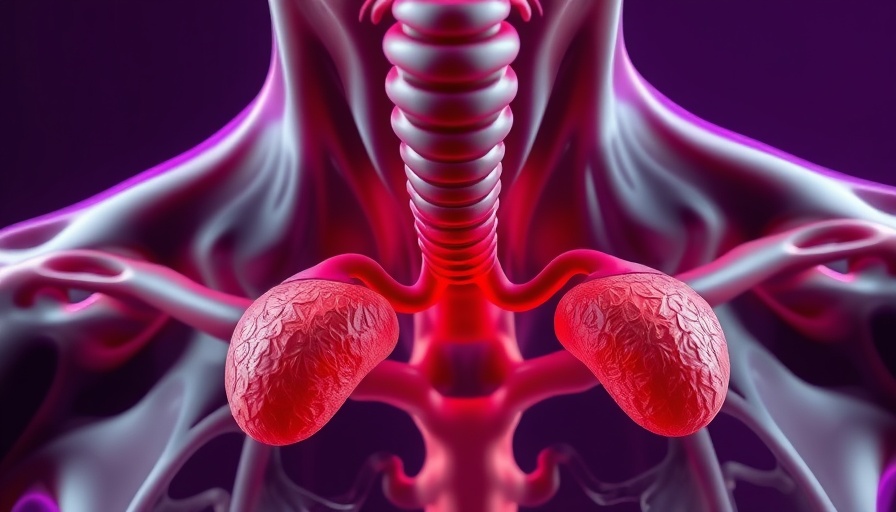
Understanding PCOS and Its Challenges for Adolescents
Polycystic ovary syndrome (PCOS) continues to be a complex condition affecting young girls, particularly those facing obesity. A recent study at the annual ENDO 2025 meeting shed light on the outcomes of bariatric surgery for adolescents with PCOS, revealing significant insights into symptom management and weight loss. While metabolic surgery is often heralded for its weight loss benefits, its role in treating the reproductive symptoms associated with PCOS remains limited, highlighting notable differences between adults and adolescents.
Key Findings from the Recent Study
This retrospective cohort study, involving 100 adolescent girls, reported that only 11% of those with PCOS achieved complete remission of their symptoms after significant weight loss post-surgery. Dr. Meghna Gaddam, an MD candidate at Northwestern University, emphasized that while 64% of participants experienced partial symptom improvement within a year, later evaluations showed all of these girls faced recurrences of either PCOS or risk factors for the condition. Furthermore, those at risk for PCOS showed no remission a year post-surgery, underscoring the nuanced challenges faced by adolescents compared to adults.
The Hormonal Landscape: Why Adolescents Are Not Just 'Small Adults'
Dr. Gaddam points out that the hormonal dynamics in adolescents differ significantly from adults. The presence of a fully developed hypothalamic-pituitary-adrenal (HPA) axis and greater hormonal variability means that the same surgical approach that yields high remission rates in adult women may not produce the same results in younger populations. As a result, the effectiveness of metabolic surgery in resolving reproductive symptoms among teenage girls requires further investigation.
Challenges in Managing PCOS in Teens
Healthcare providers see a troubling trend: despite successful weight reduction through metabolic surgery, adolescent girls often continue to grapple with hormonal imbalances. Many remain tied to their symptoms, as evidenced by a 40% incidence of new cycle irregularities in those who previously had regular menses post-surgery. The study indicates a pressing need for comprehensive long-term support and follow-up care to effectively address these persistent issues.
Current Treatment Options: Exploring the Limitations
Given the limitations of prevailing treatments—which primarily involve diet, exercise, and medications like metformin—bariatric surgery is increasingly viewed as an option when conventional methods fail. Yet, the results from the recent study signal caution. Solutions for PCOS in adolescents are not merely tethered to weight loss but necessitate a broader understanding of metabolic health and symptom management. Efforts by practitioners must emphasize tailored interventions that account for the unique needs of young patients.
The Importance of Continued Research and Education
As we venture deeper into understanding adolescent PCOS, it's essential that ongoing research continues to explore multifaceted treatment approaches. The gap in knowledge between treatments suited for adults versus those for teenagers suggests that more investigation is needed to develop accepted clinical practice guidelines. Moreover, educational initiatives targeting healthcare providers on the long-term implications of bariatric surgery for teens are essential to maximizing community health outcomes.
Conclusion: A Path Forward for Patients and Providers
While the findings from recent research provide a clearer picture of the limitations of bariatric surgery in adolescent girls with PCOS, they also open avenues for enhanced dialogue among healthcare providers and patients. Recognizing the distinct challenges this younger demographic faces is the first step toward tailoring effective interventions. As we witness the evolving landscape of adolescent PCOS management, collaboration and continual education within the medical community will be critical.
 Add Row
Add Row  Add
Add 




 Add Row
Add Row  Add
Add 

Write A Comment