Understanding Emergency Department Overcrowding: Myths and Realities
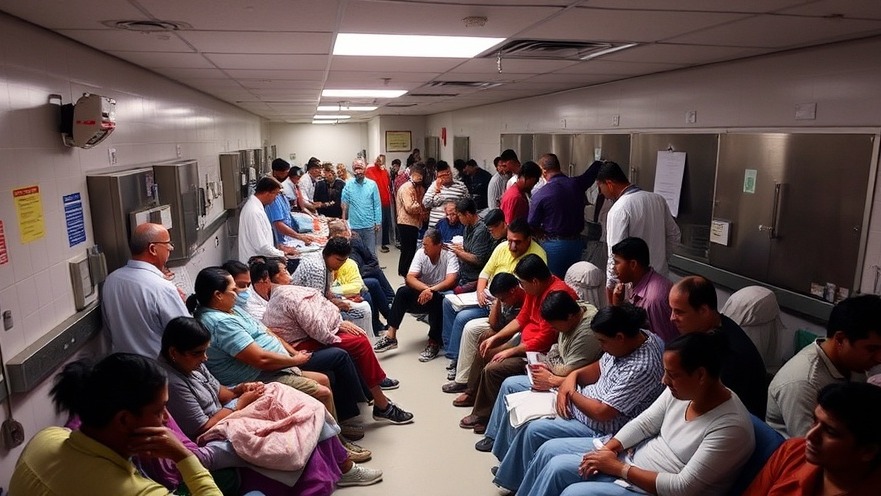
Emergency department (ED) overcrowding has long been a pressing issue in healthcare, and it often sparks heated debates among healthcare professionals. A prevalent myth is that patients with low-acuity conditions are primarily to blame for this crisis. However, leading emergency medicine experts are challenging this notion, arguing that it detracts from identifying the real systemic challenges faced by emergency departments.
The Role of Patient Demographics
As noted by Dr. Michael Bublewicz, chief medical officer of Memorial Hermann Health System, the assumption that low-acuity patients are the main contributors to ED congestion is misplaced. Recent data indicates that the demographic profile of patients visiting EDs has shifted significantly. The increasing influx of elderly patients with complex medical issues underscores a new urgent need, complicating the simplistic view of ED overcrowding.
Data from the Emergency Department Benchmarking Association shows that vulnerable groups such as the homeless and nursing home residents are utilizing emergency services at a higher rate. With our population aging, this demand is expected to rise, suggesting a more nuanced picture of healthcare delivery and service management needs.
Where to Focus Solutions: Beyond Patient Volume
Many traditional approaches to reducing ED overcrowding concentrate on managing patient flow — for example, educating patients on when to seek care at an urgent clinic instead of an ED. However, experts highlight that without addressing systemic issues, these efforts are unlikely to yield significant results. A report from the Agency for Healthcare Research and Quality emphasized the importance of understanding that simply diverting low-acuity patients away from EDs does not decrease boarding, as these patients seldom require hospitalization.
Instead, the conversations around this issue should delve deeper into the fundamental operational challenges, such as limited inpatient bed capacity and the financial models that incentivize high-revenue surgical procedures, often at the expense of general emergency care.
Economic Factors in Emergency Care
Compounding the issue are the financial incentives that many hospital systems face. Many facilities are often structured to prioritize high-revenue procedures, resulting in an unbalanced focus on surgical cases over comprehensive emergency services. This misalignment creates burdens on healthcare providers attempting to manage an influx of patients without the necessary resources and infrastructure.
Decision-makers need to explore solutions that foster broader systemic changes, such as enhancing employee health benefits or supporting independent pharmacy growth to reduce patient dependency on EDs. Exploring innovative tools and technologies like healthcare automation or practice revenue optimization techniques could help alleviate pressure on emergency rooms.
Navigating Systemic Challenges: Call to Action
Healthcare providers, policymakers, and hospital executives must come together to address these pressing challenges. By focusing on comprehensive systemic reforms and embracing collaboration across various sectors, we can shift the narrative from blaming patients for overcrowding to understanding and solving the underlying issues that truly contribute to ED boarding.
Engagement tools, digital front desk automation, and Medicare-backed services can play an essential role in improving practice workflows and efficiencies. For independent practitioners, leveraging telehealth revenue opportunities and pre-tax benefit plans can enhance patient engagement while improving overall clinic profitability.
As healthcare professionals and organizations continue to innovate and develop more effective systems, prioritizing community health and equity will not only foster a better environment for patients seeking care but also improve overall practice health. Now is the time to take these insights to heart and drive change in our health systems.
 Add Row
Add Row  Add
Add 




 Add Row
Add Row  Add
Add 

Write A Comment